Dylan Izadseta fought tirelessly to welcome a second child into her family. She pursued IVF treatments, which ultimately were successful. At the age of 39, she was filled with joy and anticipation as she eagerly planned for the arrival of her precious daughter. Throughout her pregnancy, Dylan devoted herself to nurturing and protecting her little one, showcasing the same fierce determination that had fueled her quest to conceive. Her story is a testament to the strength of a mother’s love.
Dylan faced the dual challenges of advanced maternal age and a history of pregnancy losses. It’s essential for pregnant women to consult a high-risk doctor, known as a maternal-fetal medicine specialist, if they are 35 years or older at the time of conception, as this age is deemed high-risk for pregnancy. Furthermore, those with other risk factors, such as a history of pregnancy complications, should expect to be referred and their pregnancy to be followed by a high-risk physician to ensure a safe and healthy pregnancy experience. Dylan’s OB referred her to a high-risk specialist, but only to rule out a potential Cystic Fibrosis diagnosis since Dylan is a carrier. After a second ultrasound, Dylan was told she no longer needed to see the high-risk doctor as her baby looked great. Her OB had never addressed the possibility of her pregnancy being high-risk, leaving her unaware that she should have been treated as such. This lack of communication weighed heavily on her, as she reflected on what could have been if her high-risk status had been acknowledged.
When she began experiencing pregnancy complications, Dylan found herself in the care of her nurse practitioner. She was misdiagnosed with chronic hypertension, while the reality was that she was experiencing gestational hypertension early in her pregnancy.
Dylan was eagerly yet nervously anticipating her April due date. At 38 weeks she attended her routine prenatal appointment where she underwent a five-minute stress test. During this visit, she was seen by her OB’s physician assistant (PA), who observed some concerning leakage and inquired if Dylan’s water had broken. Dylan was experiencing unsettling symptoms: arm swelling, diarrhea, and sharp cramping that began on the left side of her abdomen, gradually traveling to her right side. Concerned about her condition, she consulted her doctor, who reassured her that these complications were merely Braxton Hicks contractions and nothing to worry about. Yet the PA expressed worry that Dylan might be losing essential amniotic fluid. Recognizing the seriousness of the situation, the PA emphasized the need for closer monitoring and encouraged Dylan to stay hydrated by drinking plenty of fluids. She assured Dylan that she would arrange for her OB to order an Amniotic Fluid Index (AFI) ultrasound and additional stress tests. Although Dylan’s OB signed off on the order, the necessary tests were never carried out.
Dylan’s final appointment with her OB took place in her 40th week of pregnancy. During that visit, she underwent a stress test, yet no AFI ultrasound was performed to assess her amniotic fluid levels. The test would have revealed that Dylan was increasingly losing amniotic fluid. Without it her OB reassured her, stating that if she didn’t go into labor within four days, she should return to the office. Her doctor never discussed delivery options with her and sent her home.
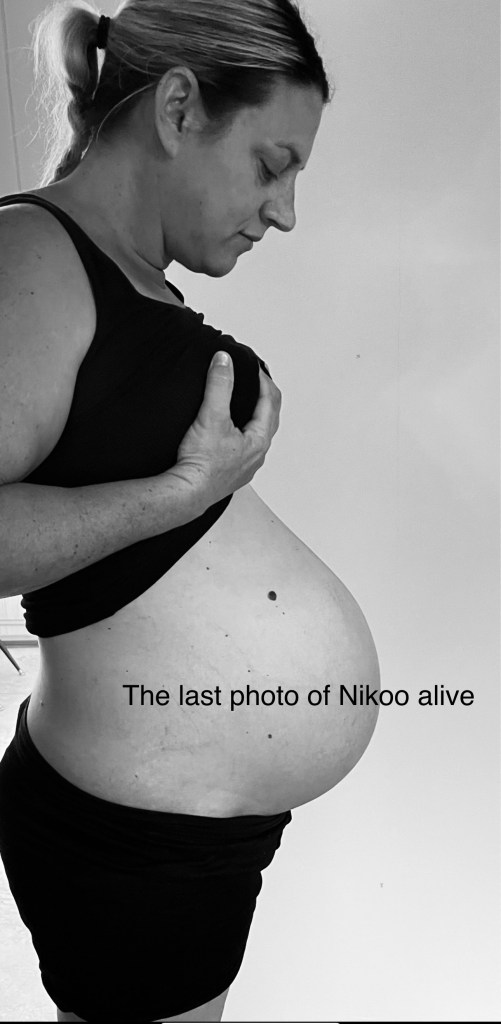
The next day she got a really bad cramp with some blood loss. Dylan called her doctor as she was starting to have contractions. She was told not to go to the hospital until she had six contractions within an hour. At that point, Dylan could barely feel her baby Nikoo moving. She went straight to the hospital. Upon arrival in labor and delivery, staff could not detect a heartbeat. An ultrasound showed baby Nikoo slumped over. During this critical time, no one spoke to her at the hospital. They would not answer her questions and kept directing her to her doctor who was nowhere to be found. No hospital physician ever came to check on her. No one would tell her if her baby girl was alive. Hospital staff would only offer her something to drink, but no one would look into her eyes. Eventually, the nurse walked into her room informing Dylan that she had her OB on the phone. Her OB was yelling at her over the phone demanding to know what happened. He asked her whether she wanted a vaginal birth or a C-section. He claimed he didn’t have the results from her ultrasound but later admitted that her baby was deceased.
Dylan spent the entire day in the hospital, in her hospital bed, enveloped in deep sorrow for her precious baby girl. As the clock struck 5 PM, the nursing director entered the room. She told Dylan, “I am sorry for your loss,” she conveyed. “This is not your doctor’s fault; it is no one’s fault.” Dylan felt a wave of despair wash over her, still awaiting her doctor to deliver the baby she had longed for so long.
At around 6 PM, her doctor rushed into the room. He said, “I don’t know what happened; this hasn’t happened to me in 15 years,” he admitted. He revealed that there was a tiny puncture that no one could have detected. Yet, his physician’s assistant had foreseen trouble, warning him that Dylan was leaking amniotic fluid and recommending AFT ultrasounds. Unfortunately, the doctor did not follow through to ensure Dylan received the necessary ultrasounds, leaving her baby with zero amniotic fluid. Tragically, baby Nikoo died of acute sepsis, which was passed on to Dylan.
Dylan continued to wait in her hospital bed, with increasing anxiety. At 12:50 AM, her doctor burst into the room, brimming with enthusiasm, clapping his hands as he declared, “Let’s have a baby!” As he performed an episiotomy, he sliced baby Nikoo’s delicate face twice with the scissors leaving her precious face cut below and above her eye. He placed baby Nikoo on Dylan’s chest while he stitched her up. Upon completion, he turned to Dylan’s husband, telling him, “Look at that vagina. It’s as good as new!” In that moment, Dylan remained lost in her grief, her heart heavy with disbelief as she memorized the haunting image of her baby’s injured face.
Dylan was not only fighting a fierce battle against acute sepsis but also grappling with the profound grief of losing her beautiful baby girl. Amidst this heart-wrenching sorrow, the hospital and doctor were trying to protect themselves from liability. She was stunned to learn that the Director of Nursing had reached out to them twice, even leaving a voicemail for her husband. In an urgent tone, the Nursing Director insisted on the necessity of meeting with the doctor that weekend, asserting that Dylan’s physician bore no responsibility for the tragic death of baby Nikoo.
In the wake of the heartbreaking loss of baby Nikoo, Dylan took action by contacting the medical board to file a consumer complaint against her OB. The investigation into baby Nikoo’s case is ongoing and has revealed a troubling pattern of medical negligence by the same doctor. Dylan has connected with numerous families who share similar harrowing experiences, and another mother has also bravely stepped forward to file her own complaint with the medical board against the same doctor.
Dylan has joined Consumer Watchdog’s advocacy team to champion vital reforms in our medical boards, elevate awareness around maternal mortality, and shine a light on the important issue of stillbirth.


