Myth #1: Legal Restrictions on Victims Lowered California Doctors’ Malpractice Premiums.
Facts: Californians enacted the strongest insurance rate regulation in the nation in 1988 through insurance reform Proposition 103 (Prop 103), a ballot initiative passed by the voters and authored by Consumer Watchdog founder Harvey Rosenfield. This law resulted in a rate freeze, a rate rollback, and stringent regulation that reduced premiums in all lines of insurance — including medical malpractice.
In 1975, California enacted a series of legal restrictions on injured patients — the Medical Injury Compensation Reform Act (MICRA). Data from the National Association of Insurance Commissioners, summarized in graphs linked to below show that:
- Overall, California medical malpractice premiums increased dramatically during the first thirteen years with MICRA and substantially decreased after voters’ approved Proposition 103. (See graph)
- Medical malpractice premiums remained extremely volatile after MICRA and did not stabilize until Prop 103 imposed rate regulation in 1988.
- In 1986, after a decade of MICRA, California was once again mired in an insurance crisis, with medical malpractice premiums rising at a rate of 26% annually, faster than premiums rose nationally during the same period. In fact, the year MICRA’s cap of damages was upheld in court (1985), California malpractice premiums increased by 20% and the following year rates jumped an additional 40%.
- Conversely, after three years of insurance regulation under Prop 103, medical malpractice rates had fallen by more than 20%. During the first decade of regulation, premiums were down by 7% and, if we adjust for inflation, medical malpractice premiums are down by 35% since the enactment of regulation.
- California medical malpractice premiums tracked closely with national trends until Proposition 103 set California apart, by statutorily requiring lower insurance rates. (See graph)
Former Governor Jerry Brown, who signed the MICRA law, stated seventeen years later (on June 13, 1993) that he would not recommend it for the nation because in the interlude he “witnessed yet another insurance crisis and found that insurance company avarice, not utilization of the legal system by injured consumers was responsible for excessive premiums.” “Saddest of all,” Brown continued, is “the arbitrary and cruel effect upon victims of malpractice.” (Read Brown’s full statement)
Myth #2: Injured patients are still able to hold wrongdoers legally accountable because only “non-economic” damages are capped — compensation for those damages not measured by wage loss, medical bills, or other tangible economic measures.
Facts: Only those patients with large wage loss or medical bills are typically able to find attorneys in California. Most medical malpractice victims cannot. For example, injured patients who, as a result of medical negligence, lose their fertility or are severely disfigured typically cannot prove “economic” damage. Similarly, the death of a child or senior citizen typically does not result in “economic” damage because there is no basis for wage loss or measuring medical bills. In these types of California cases, there is typically no legal accountability for wrongdoers.
The situation stirred well-known insurance defense attorney Robert Baker, who defended malpractice suits for more than twenty years, to tell Congress about the problem. “In my view, these malpractice reforms have aided insurance companies and physicians, but have, to a significant extent, been detrimental to person injured by medical negligence,” Baker testified before the House Judiciary Committee in 1994 on behalf of the American Board of Trial Advocates (ABOTA). “As a result of the caps on damages, most of the exceedingly competent plaintiff’s lawyers in California simply will not handle a malpractice case.
“There are entire categories of cases that have been eliminated since malpractice reform was implemented in California. The victims of cases that have a value between $50,000 and $150,000 are basically without representation. As an example, incidents of failure to diagnose an appendicitis still occur, but suits are not filed to any extent in California.”
Soon after the testimony, Baker’s major clients — the HMO Kaiser Permanente and malpractice insurer The Doctors’ Company — fired him. (Read Baker’s full statement)
Legal fees and expenses are not added on to the “economic” damage award, so they must be subtracted from the capped “non-economic” damages portion. This makes expensive cases without significant economic damage components not viable for attorneys.
Myth #3: A one-size-fits-all cap on compensation is fair to patients who can receive “unlimited” economic damages.
Facts: Economic damages cannot always be anticipated. California juries are not informed of the cap on non-economic damages, so they are often not careful about apportioning economic damages. In one famous case, for example, Harry Jordan, a Long Beach man, was hospitalized to have a cancerous kidney removed but the surgeon took out his healthy kidney instead. A jury awarded Jordan more than $5 million dollars, but the judge was required to reduce the verdict to $250,000 due to California’s cap on “non-economic” damages – plus a mere $6,000 in “economic costs”. Jordan, who lived for years on 10% kidney function, could no longer work, though the jury (which lawfully cannot be notified about the “non-economic” cap) did not take this into account. Jordan’s court costs — not including attorney fees — amounted to more than $400,000 and his medical bills, that arose after frequently being denied by insurers, totaled more than $500,000. He paid $1700 per month in health insurance.
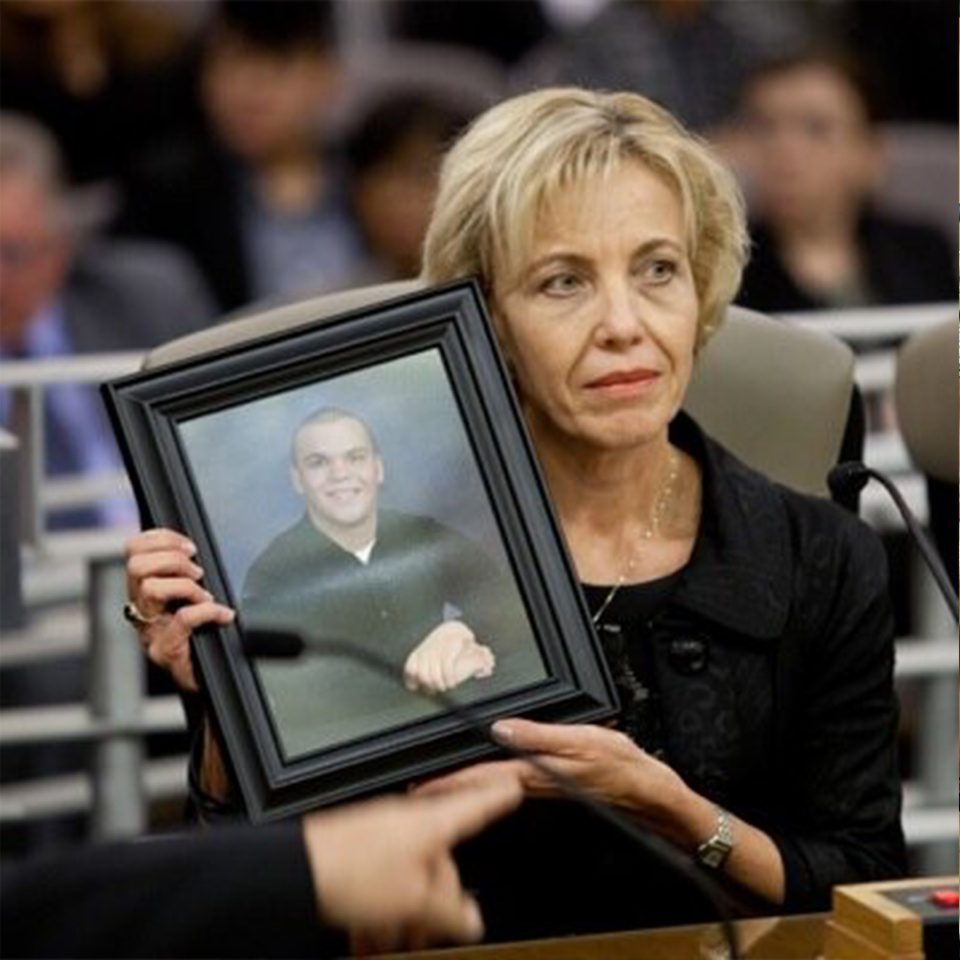
The stories of other patients victimized by California’s restrictions can be found in FTCR’s testimony before Congress.
Read a letter from members of California’s Congressional Delegations critical of MICRA.
Myth #4: Malpractice damage caps are about doctors vs. lawyers .
Facts: Malpractice caps are about patients vs. reckless HMOs and managed care corporations.
Twelve years old today, Steven Olsen is blind and brain damaged because, as a jury ruled, he was a victim of medical negligence when he was two years old. He fell on a stick in the woods while hiking. Under the family’s HMO plan, the hospital pumped Steven up with steroids and sent him away with a growing brain abscess, although his parents had asked for a CAT scan because they knew Steven was not well. The next day, Steven Olsen came back to the hospital comatose. At trial, medical experts testified that had he received the $800 CAT scan, which would have detected a growing brain mass, he would have his sight and be perfectly healthy today.
The jury awarded $7.1 million in “non-economic” damages for Steven’s avoidable life of darkness and suffering. However, the jury was not told of the two decade old restriction on non-economic damages in the state. The judge was forced to reduce the amount to $250,000. The jurors only found out that their verdict had been reduced by reading about it in the newspaper. Jury foreman Thomas Kearns expressed his dismay in a letter published in the San Diego Union Tribune.
“We viewed video of Steven, age 2, shortly before the accident. This beautiful child talked and shrieked with laughter as any other child at play. Later, Steven was brought to the court and we watched as he groped, stumbled and felt his way along the front of the jury box. There was no chatter or happy laughter. Steven is doomed to a life of darkness, loneliness and pain. He is blind, brain damaged and physically retarded. He will never play sports, work, or enjoy normal relationships with his peers. His will be a lifetime of treatment, therapy, prosthesis fitting and supervision around the clock. . . Our medical-care system has failed Steven Olsen, through inattention or pressure to avoid costly but necessary tests. Our legislative system has failed Steven, bowing to lobbyists of the powerful American Medical Association (AMA) and the insurance industry, by the Legislature enacting an ill-conceived and wrongful law. Our judicial system has failed Steven, by acceding to this tilting of the scales of justice by the Legislature for the benefit of two special- interest groups. . .. I think the people of California place a higher value on life than this.”
In 2001, Steven had 74 doctor visits, 164 physical and speech therapy appointments, and three trips to the emergency room. And his parents say that was a good year because Steven was not hospitalized. Steven’s mother Kathy had to leave her job because caring for Steven is a full time job. She has to struggle constantly with the school district for Steven to receive special education classes. One day, Steven ate part of a light bulb, not an uncommon problem for children with brain injuries. He has to be watched constantly. Insurance executives that seek to limit jury awards for the individual’s pain and suffering claim society must do so to save money. Yet these executives typically make millions every year without any of Steven Olsen’s pain and suffering. Limiting their responsibility for the pain of individuals reduces not only the corporation’s accountability, but the worth of the individual to that of a mere object.
Kathy Olsen said this about Steven: “It has been 10 years ago this month when Steven came home from a 5-month life changing stay at the hospital. He was only 2 years old. When he went into the hospital no one asked his party affiliation. He was a casualty of the system. The system that he had no say in. Which lawmakers were looking out for him? Now with all his disabilities he will never see, do things that the average person gets to do in their lifetime, or vote in an election. Please look out for all the Steven Olsens in this great country. Don’t let this happen over and over again.”
Myth #5: Defensive medicine is always bad, significantly drives up the costs of medicine and results from doctors facing full legal accountability.
Facts: In the managed care age, the financial incentives point the other way — to less caution, not more. Proponents of limiting victims’ rights claim that doctors’ fear of lawsuits, so called defensive medicine, is driving them to perform unnecessary tests and procedures.
The Congressional Office of Technology Assessment foresaw this trend in July 1994, reporting that less than 8 percent of diagnostic procedures are likely to be caused by conscious concern about malpractice liability. “Defensive medicine is not always bad for patients,” the agency stated. “Malpractice reforms that remove incentives to practice defensively, without differentiating between appropriate and inappropriate defensive medicine, could also remove a deterrent to providing too little care at the very time that such mechanisms are needed.”